Welcome to our journey towards better health and happiness!
Meet Mrs. Ananya, a strong homemaker who’s been dealing with Irritable Bowel Syndrome (IBS) for twelve years. Through her story, we’ll explore how what we eat and how we live affect our well-being.
Let’s uncover the secrets of IBS and learn how nutrition and lifestyle shape our health. Join us on this adventure where every step brings us closer to understanding and thriving.
Background:
Mrs. Ananya’s life is a testament to the intricate dance between health and daily habits. Despite experiencing symptoms of IBS for over a decade, she never prioritized healing or understanding the root causes of her discomfort. Her routine is characterized by familial responsibilities, occasional migraines, persistent acidity, and a series of dietary choices that inadvertently exacerbate her condition.
Triggers and Lifestyle Factors:
Ananya’s eating patterns, such as consuming leftover foods, barely eating anything during menstruation, and inadequate water intake, play a pivotal role in triggering her IBS symptoms. Moreover, stress within the family and concerns regarding her children further compound her gastrointestinal issues. These factors collectively contribute to a vicious cycle of discomfort and disquietude in her daily life.
Ananya’s struggles with Irritable Bowel Syndrome (IBS) include:
- Abdominal Discomfort: Characterized by cramping, bloating, and a persistent sense of fullness, often triggered by certain foods or stressful situations.
- Flatulence: Experiencing excessive gas production accompanied by bloating and abdominal distension, leading to embarrassment and social discomfort.
- Alternating Constipation and Diarrhea: Periods of constipation with difficulty passing stools and infrequent bowel movements, alternating with episodes of diarrhea marked by loose stools and urgency.
- Fatigue: Persistent tiredness and decreased energy levels despite adequate rest, contributing to lethargy and diminished motivation.
- Brain Fog: Cognitive symptoms such as difficulty concentrating, memory lapses, and mental sluggishness, impacting daily tasks and interactions.
Collectively, these symptoms paint a comprehensive picture of the challenges faced by individuals living with IBS, including Ananya. The multifaceted nature of these manifestations underscores the complex interplay between gastrointestinal symptoms, psychological well-being, and overall quality of life in managing this chronic condition. Addressing these symptoms holistically through a combination of dietary modifications, lifestyle interventions, and targeted therapies is essential to improving Ananya’s symptoms and enhancing her overall well-being.
Exploring the Culprits:
The blog dissects the detrimental impact of certain dietary elements on Ananya’s condition. It emphasizes the significance of maintaining a balance between complex and simple carbohydrates, incorporating good fats and proteins while eliminating potential triggers like gluten and lactose. Furthermore, it elucidates how habits such as smoking, alcohol consumption, and a hectic work schedule can exacerbate IBS symptoms, manifesting as diarrhea or constipation.
Management Strategies:
Ananya’s journey towards managing IBS begins with a personalized low FODMAP diet plan, tailored to her lifestyle and specific dietary needs. A low FODMAP diet involves reducing or eliminating foods high in these fermentable carbohydrates to alleviate symptoms of IBS. The diet typically involves three phases: elimination, reintroduction, and personalization.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates and sugar alcohols that are poorly absorbed in the small intestine and can ferment in the large intestine, leading to symptoms such as gas, bloating, abdominal pain, and altered bowel habits in individuals with irritable bowel syndrome (IBS) or other gastrointestinal disorders
| High FODMAP Foods: | Low FODMAP Foods: |
| Fruits: Apple Pears Mangoes Watermelons Cherries | Fruits: Bananas Blueberries Strawberries Grapes Kiwi |
| Vegetables: Onions Garlic Cauliflower Mushrooms Asparagus | Vegetables: Carrots Bell peppers Spinach Zucchini Potatoes |
| Grains: Wheat products (chapati, paratha) Barley (jau) Rye (salya) Wheat-based cereals (wheat flakes) | Grains: Rice (white, brown) Quinoa Oats (gluten-free) Corn (makai) Millet (bajra, jowar) |
| Legumes: Lentils (masoor dal, chana dal) Chickpeas (chana) Black beans (rajma) Kidney beans (rajma) | Proteins: Chicken Turkey Fish (salmon, trout, tuna) Eggs Tofu (firm) Soybeans (soya chunks) |
| Dairy: Milk (cow, goat) Ice cream Soft cheeses (paneer, cottage cheese) | Dairy Alternatives: Lactose-free milk Almond milk Coconut milk (in moderation) Hard cheeses (cheddar, mozzarella) |
| Sweeteners: Honey High fructose corn syrup Jaggery Sorbitol Mannitol | Fats and Oils: Ghee (clarified butter) Coconut oil Mustard oil Olive oil Butter (lactose-free) |
| Nuts and Seeds: Cashews Pistas | Nuts and Seeds (in moderation): Almonds (badam) Walnuts (akhrot) Pumpkin seeds (kaddu ke beej) Sunflower seeds (soorajmukhi ke beej) |
Adjustments may still be needed based on individual tolerance and regional variations in ingredients. It’s advisable to work with a healthcare provider or registered dietitian when implementing a low FODMAP diet. This ensures proper implementation, monitoring, and individualized guidance throughout the process to optimize symptom relief and nutritional balance.
Additionally, the low FODMAP diet is not intended to be a lifelong restriction but rather a short-term intervention to identify trigger foods and develop a personalized dietary approach for managing IBS symptoms.
Importance of a Dietitian in the Process:
- Personalization: A dietitian can personalize a low FODMAP diet based on individual needs, considering factors like food preferences, cultural considerations, and lifestyle.
- Education: Dietitians provide education about FODMAPs, IBS triggers, and how to effectively manage symptoms through dietary modifications.
- Monitoring: Dietitians can monitor progress and make necessary adjustments to the diet plan to ensure it’s effective and sustainable.
- Nutritional Balance: They ensure that despite dietary restrictions, individuals are still receiving adequate nutrition to support overall health.
- Behavioral Support: Dietitians offer support and guidance to help individuals navigate social situations, dine out, and manage stress-related eating habits, which can all impact IBS symptoms.
- Long-term Management: Dietitians assist in creating a long-term plan for managing IBS symptoms, promoting dietary diversity once symptoms are under control, and reintroducing certain foods.
- Collaboration: Dietitians often collaborate with other healthcare professionals, such as gastroenterologists or therapists, to provide comprehensive care for individuals with IBS.
Hydration plays a crucial role in supporting digestive health, and it is particularly important for managing both diarrhea and constipation effectively.
Diarrhea: | Constipation: |
During episodes of diarrhea, the body loses fluids rapidly through increased frequency of bowel movements. This loss of fluids can lead to dehydration if adequate hydration is not maintained. Dehydration can exacerbate symptoms such as fatigue, weakness, dizziness, and electrolyte imbalances, further compromising overall health and well-being. | In contrast, adequate fluid intake is equally important for managing constipation. Dehydration can contribute to the hardening of stools and difficulty passing bowel movements, exacerbating symptoms of constipation. Insufficient hydration can also lead to reduced motility in the gastrointestinal tract, making it harder for stools to move through the colon and leading to further constipation. |
| The importance of fluid intake during diarrhea management cannot be overstated. Adequate hydration helps replenish lost fluids, maintains electrolyte balance, and supports the body’s natural processes of fluid absorption in the intestines. Drinking plenty of fluids, such as water, electrolyte-rich beverages (e.g., sports drinks, coconut water), clear broths, and herbal teas, can help replace lost fluids and prevent dehydration. | By increasing fluid intake, particularly water, individuals with constipation can help soften stools, promote regular bowel movements, and alleviate discomfort associated with constipation. Drinking water throughout the day helps maintain hydration levels, supports digestive function, and ensures optimal stool consistency for easier passage. |
Overall, maintaining adequate fluid intake is essential for supporting digestive health and managing symptoms of both diarrhea and constipation. By prioritizing hydration and consuming a variety of fluids throughout the day, individuals can promote optimal bowel function, alleviate discomfort, and support overall well-being.
Alternative strategies such as affirmations, guided meditation, and nature baths offer additional tools for managing stress and promoting relaxation, which can be beneficial for individuals with irritable bowel syndrome (IBS) or other gastrointestinal disorders:
Affirmations: Positive statements or phrases repeated regularly to reinforce a desired mindset or belief. Ananya can use affirmations to cultivate a positive outlook, reduce anxiety, and enhance self-confidence in managing her IBS symptoms.
Guided Meditation: Involves listening to a trained instructor or recorded audio that leads participants through relaxation techniques, visualization exercises, and mindfulness practices. This practice of guided meditation can promote relaxation, reduce stress, and soothe gastrointestinal symptoms.
Nature Baths: Immersing oneself in natural environments such as forests, parks, or gardens to reduce stress, improve mood, and enhance overall well-being. One can benefit from spending time in nature to lower cortisol levels, reduce inflammation, and improve gastrointestinal health.
These alternative strategies complement conventional treatments and dietary modifications, providing a comprehensive approach to managing symptoms and improving quality of life.
The Gut-Brain Axis and Holistic Health:
Central to Ananya’s journey is an exploration of the gut-brain axis and its profound influence on mood, behavior, and overall well-being.
Let us understand the Gut-Brain Axis:
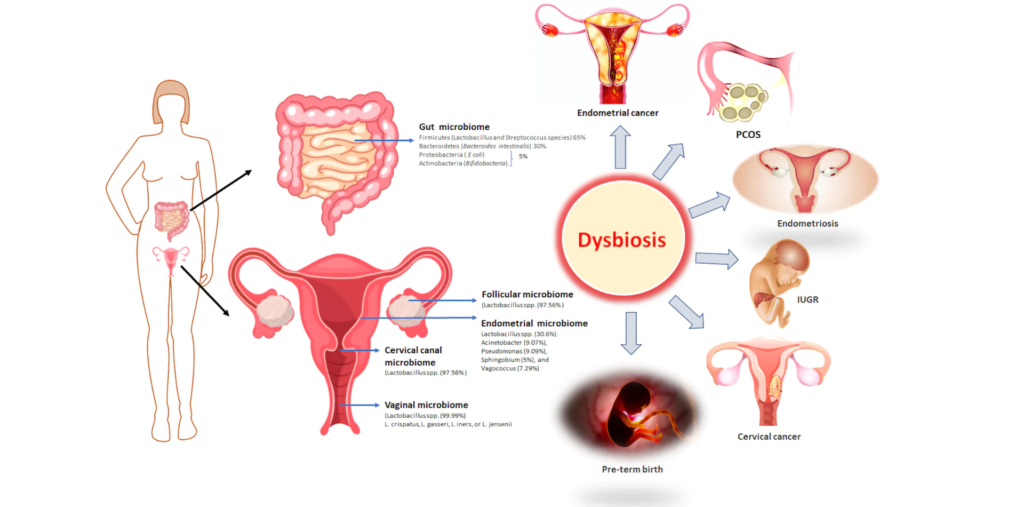
The gut-brain axis represents a bidirectional communication system between the gastrointestinal tract and the central nervous system. It involves complex interactions between the gut microbiota, intestinal mucosa, immune system, and the brain. This intricate network not only regulates digestion but also influences various physiological processes, including mood, cognition, and behavior.
Impact on Mood and Behavior:
Research has shown that alterations in gut microbiota composition can impact neurotransmitter production and signaling pathways, thereby influencing mood and behavior. In Ananya’s case, the imbalance in her gut microbiome due to prolonged IBS symptoms could potentially contribute to feelings of anxiety, stress, and irritability, further exacerbating her gastrointestinal issues. Understanding this connection underscores the importance of nurturing a healthy gut microbiome for emotional well-being.
The Role of Sleep Hygiene and Circadian Rhythms:
Maintaining good sleep hygiene and synchronizing with the body’s natural circadian rhythms play a pivotal role in supporting gut health and hormonal balance. Adequate sleep duration and quality are essential for the maintenance of a diverse and resilient gut microbiome.
Disruptions in sleep patterns, such as irregular sleep schedules or sleep deprivation, can negatively impact gut health and exacerbate gastrointestinal symptoms. By prioritizing sleep hygiene and aligning with the body’s natural rhythms, individuals can support their overall health and well-being.
Preventing Metabolic and Hormonal Disorders:
A healthy gut microbiome acts as a barrier against metabolic disorders such as obesity, diabetes, and insulin resistance. The gut microbiota plays a crucial role in energy metabolism, nutrient absorption, and the regulation of appetite and satiety hormones. By nurturing a diverse and balanced gut microbiome through dietary interventions and lifestyle modifications, individuals can mitigate the risk of metabolic disorders and maintain hormonal balance.
Here are some interventions individuals can make to nurture a diverse and balanced gut microbiome:
- Dietary Modifications: Incorporating a variety of fiber-rich foods such as fruits, vegetables, whole grains, legumes, and nuts can promote the growth of beneficial gut bacteria. Fermented foods like yogurt, kefir, kimchi, sauerkraut, and kombucha are also rich sources of probiotics, which contribute to a healthy gut microbiome.
- Prebiotics: Consuming prebiotic-rich foods like onions, garlic, leeks, asparagus, bananas, and oats can serve as fuel for beneficial gut bacteria, promoting their growth and activity.
- Limiting Processed Foods: Minimizing intake of processed and sugary foods can help prevent the proliferation of harmful bacteria in the gut, thereby preserving microbial balance.
- Reducing Antibiotic Use: Whenever possible, avoiding unnecessary or prolonged antibiotic use can help prevent disruption of the gut microbiome. If antibiotics are necessary, pairing them with probiotics may help mitigate their negative impact on gut health.
- Stress Management: Engaging in stress-reducing activities such as mindfulness meditation, deep breathing exercises, yoga, and spending time in nature can help modulate the gut-brain axis and promote a healthy gut microbiome.
- Adequate Sleep: Prioritizing good sleep hygiene and ensuring adequate, quality sleep can support the body’s natural circadian rhythms, which are closely linked to gut health and hormonal balance.
- Regular Physical Activity: Incorporating regular exercise into one’s routine can have beneficial effects on gut microbial diversity and overall metabolic health.
- Hydration: Maintaining adequate hydration by drinking plenty of water throughout the day supports digestive function and helps flush out toxins, contributing to a healthy gut environment.
By implementing these interventions, individuals can cultivate a thriving gut microbiome, promoting not only digestive health but also overall well-being and resilience against metabolic and hormonal disorders.
The Unique Challenges for Women:
Given the fluctuating hormonal landscape that women navigate throughout the month, the blog underscores the heightened importance of mindful food choices for female gastrointestinal health. It delineates how hormonal shifts can exacerbate bowel issues, necessitating a nuanced approach towards nutrition and self-care.
- Cycle Tracking: Women can track their menstrual cycle to anticipate hormonal fluctuations and adjust their diet and lifestyle accordingly. This proactive approach can help them manage bowel issues more effectively.
- Nutrient Timing: Being mindful of nutrient timing during different phases of the menstrual cycle can be beneficial. For example, focusing on iron-rich foods during menstruation to replenish lost nutrients and incorporating magnesium-rich foods during the premenstrual phase to alleviate symptoms like bloating and constipation.
- Herbal Support: Exploring herbal remedies such as ginger or peppermint tea to soothe gastrointestinal discomfort during hormonal fluctuations can offer natural relief without interfering with gut microbiome balance.
- Hydration Strategies: Women can implement hydration strategies tailored to their menstrual cycle, such as increasing water intake during the premenstrual phase to counteract fluid retention and minimize bloating.
- Mindful Eating Practices: Practicing mindful eating techniques specific to hormonal fluctuations, such as paying attention to cravings and hunger cues, can help women make informed food choices that support digestive health throughout the month.
- Supplementation: Consider targeted supplements like calcium or vitamin D to support overall hormonal balance and alleviate gastrointestinal symptoms.
The Consequences of Neglect:
Ananya’s journey serves as a cautionary tale, highlighting the potential ramifications of neglecting gut health. Left unchecked, IBS can progress to more severe conditions. Let us learn about the consequences.
Neglecting Irritable Bowel Syndrome (IBS) can have a range of consequences that extend beyond gastrointestinal discomfort.
- Worsening Symptoms: Ignoring IBS symptoms and failing to address underlying triggers can lead to a worsening of gastrointestinal symptoms such as abdominal pain, bloating, diarrhea, and constipation. Over time, these symptoms may become more frequent and severe, significantly impacting daily life and overall well-being.
- Psychological Distress: Chronic gastrointestinal symptoms can take a toll on mental health, contributing to increased levels of anxiety, depression, and stress. The constant discomfort and unpredictability of symptoms may lead to social withdrawal, decreased quality of life, and impaired work or academic performance.
- Nutritional Deficiencies: Persistent gastrointestinal issues can interfere with nutrient absorption, leading to deficiencies in essential vitamins, minerals, and nutrients. Over time, this can compromise overall health and increase the risk of other medical conditions related to malnutrition.
- Complications: Neglected IBS may predispose individuals to various complications such as intestinal inflammation, diverticulitis, hemorrhoids, and anal fissures. These complications can further exacerbate symptoms and require medical intervention to manage effectively.
- Impact on Quality of Life: Untreated IBS can significantly diminish the quality of life, affecting various aspects such as relationships, social activities, and emotional well-being. The constant struggle with symptoms and their unpredictable nature can lead to feelings of frustration, isolation, and hopelessness.
- Increased Healthcare Costs: Neglecting IBS may result in frequent medical consultations, diagnostic tests, and medications to manage symptoms and complications. The cumulative healthcare costs associated with untreated IBS can be substantial over time, placing a financial burden on individuals and healthcare systems.
- Risk of Serious Conditions: Long-term neglect of IBS may elevate the risk of developing more serious gastrointestinal conditions such as inflammatory bowel disease (IBD), colorectal cancer, and metabolic disorders like obesity and type 2 diabetes. These conditions often require more aggressive treatment strategies and can have significant implications for long-term health outcomes.
Through Mrs. Ananya’s narrative, we glean insights into the multifaceted nature of Irritable Bowel Syndrome and the pivotal role of nutrition, lifestyle modifications, and holistic wellness practices in its management. As we navigate the complexities of gastrointestinal health, may Ananya’s journey inspire us to prioritize self-care, nurture our bodies, and embrace a path toward sustainable nutrition and well-being.
While you are at it, let us provide you with some functional foods that would help alleviate some of your symptoms-
In irritable bowel syndrome (IBS), psyllium husk, a soluble fiber, can:
- Relieve Constipation: Absorbs water softens stools and promotes regular bowel movements, especially beneficial for IBS-C.
- Regulate Bowel Movements: Adds bulk to stools, improving consistency, and alleviating symptoms of both constipation and diarrhea.
- Alleviate Bloating and Gas: Helps prevent gas buildup in the digestive tract, reducing bloating and discomfort.
- Support Gut Health: Acts as a prebiotic, nourishing beneficial gut bacteria and fostering a healthy gut environment.
- Enhance Satiety and Weight Management: Increases feelings of fullness, aiding in weight management and portion control.
While psyllium husk is commonly used to alleviate constipation, it’s important to note that it may not suit everyone. Certain individuals may experience adverse effects or contraindications, emphasizing the need for individualized recommendations. An expert’s guidance is essential to determine the suitability of psyllium husk and explore alternative options if necessary.
Let us look at foods that can help alleviate symptoms of constipation and diarrhea:
Constipation:
- Prunes: Prunes are high in fiber and contain sorbitol, a natural laxative that can help soften stools and promote bowel movements.
- Flaxseeds: Flaxseeds are rich in fiber and omega-3 fatty acids, which can help bulk up stools and promote regularity.
- Chia Seeds: Chia seeds are packed with fiber and can absorb water, forming a gel-like substance that helps soften stools and ease constipation.
- Kiwi: Kiwi is high in fiber and contains actinidin, an enzyme that aids in digestion and may help alleviate constipation.
- Leafy Greens: Vegetables like spinach, kale, and broccoli are excellent sources of fiber and magnesium, which can help regulate bowel movements and relieve constipation.
- Oatmeal: Oatmeal is a fiber-rich whole grain that can help add bulk to stools and promote regularity.
- Apples: Apples are high in fiber, particularly soluble fiber called pectin, which can help soften stools and alleviate constipation.
Diarrhea:
- Bananas: Bananas are easily digestible and contain pectin, which can help absorb excess fluid in the intestines and firm up stools during diarrhea.
- White Rice: Plain white rice is gentle on the stomach and can help bulk up stools and reduce the frequency of bowel movements during diarrhea.
- Toast: Plain toast made from white bread or whole-grain bread can help absorb excess fluid in the intestines and provide a bland, easily digestible option during diarrhea.
- Boiled Potatoes: Boiled potatoes are low in fiber and easy to digest, making them a suitable option to help settle the stomach during diarrhea.
- Yogurt: Yogurt contains probiotics, which are beneficial bacteria that can help restore the balance of gut flora and alleviate diarrhea.
- Stock: Chicken/vegetable stock is rich in electrolytes and easy to digest, making it a hydrating option to replenish lost fluids during diarrhea.
- Applesauce: Applesauce is low in fiber and can help bulk up stools and provide relief from diarrhea.
It’s important to note that individual tolerance to these foods may vary, so it’s best to introduce them gradually and observe how your body responds.
In conclusion, if you’re struggling with irritable bowel syndrome (IBS), incorporating strategies like dietary modifications, lifestyle changes, and supplements can significantly improve symptoms and enhance your quality of life. However, it’s crucial to seek personalized guidance and support from a healthcare professional to ensure the most effective management plan tailored to your individual needs.
At Nutrition with Vibha, we specialize in addressing digestive health issues like IBS through comprehensive consultations and personalized nutrition plans. With our expertise and guidance, you can take proactive steps toward resolving your IBS symptoms and achieving lasting relief. Don’t let IBS hold you back from living your best life, schedule a consultation with us today and embark on your journey toward digestive wellness.

